Practice Management: Enhance Patient Engagement Now

Welcome, to HS MED Solutions Top 5 Strategies for Effective Practice Management and Communication In today’s fast-paced healthcare environment, effective practice management and communication are crucial for maintaining a thriving medical practice. Improving these areas not only enhances patient engagement but also ensures smoother operations and optimized revenue cycle management. At HS MED Solutions, we understand the challenges healthcare providers face and offer comprehensive medical billing solutions to help practices run more efficiently. In this article, we will explore the top 5 strategies for boosting patient engagement through effective practice management and healthcare communication. Implement Advanced Medical Billing Solutions Effective practice management begins with streamlining your medical billing processes. Advanced medical billing solutions play a pivotal role in reducing errors, improving cash flow, and enhancing the overall efficiency of your practice. By automating billing tasks, practices can significantly cut down on administrative time and minimize the risk of human errors, ensuring that claims are processed accurately and promptly. Automated medical billing systems offer numerous benefits: Improved Billing Accuracy: Automated systems help reduce coding errors and ensure that claims are submitted correctly the first time. Faster Reimbursement: Streamlined processes lead to quicker claim submissions and faster reimbursements, improving your practice’s cash flow. Reduced Administrative Burden: Automation frees up staff time, allowing them to focus on patient care and other critical tasks. At HS MED Solutions, our cutting-edge billing solutions are designed to meet the unique needs of healthcare providers, ensuring that your billing processes are as efficient and accurate as possible. By leveraging our expertise and technology, you can enhance your practice’s financial stability and devote more time to what matters most—providing exceptional patient care. Enhance Patient Communication Channels Maintaining open and effective communication channels with patients is essential for fostering trust, improving patient engagement, and ensuring the smooth operation of your practice. In today’s digital age, patients expect timely and convenient communication, whether it’s for appointment reminders, test results, or billing inquiries. Here are key strategies to enhance patient communication: Multi-Channel Communication: Utilize various platforms such as email, SMS, patient portals, and even social media to communicate with patients. This ensures that you can reach patients through their preferred methods. Automated Appointment Reminders: Implement automated systems to send reminders for upcoming appointments. This helps reduce no-shows and keeps your schedule running smoothly. Patient Portals: Provide patients with access to an online portal where they can view their medical records, communicate with their healthcare providers, and manage appointments. This empowers patients to take an active role in their healthcare. Two-Way Communication: Encourage patients to ask questions and provide feedback through secure messaging systems. This can improve patient satisfaction and help identify areas for improvement in your practice. Effective communication not only enhances patient engagement but also contributes to better health outcomes by keeping patients informed and involved in their care. At HS MED Solutions, we offer advanced communication tools integrated with our medical billing solutions to help you maintain strong patient relationships and improve practice efficiency. Optimize Practice Workflow and Scheduling Efficient practice workflow and scheduling are crucial for maximizing the productivity and effectiveness of your healthcare practice. By optimizing these areas, you can ensure that your practice runs smoothly, reduce patient wait times, and enhance the overall patient experience. Here are some strategies to optimize your practice workflow and scheduling: Automated Scheduling Systems: Implement automated scheduling software that allows patients to book appointments online. This reduces the administrative burden on your staff and provides patients with the convenience of booking appointments at any time. Streamlined Workflow Processes: Evaluate and streamline your current workflow processes to eliminate bottlenecks and inefficiencies. This could involve reassigning tasks, improving communication among staff, or adopting new technologies to automate repetitive tasks. Efficient Patient Check-In: Use digital check-in systems to speed up the patient check-in process. Patients can complete necessary forms and provide information electronically, reducing wait times and ensuring that appointments start on time. Effective Staff Utilization: Ensure that your staff is utilized effectively by assigning tasks based on their skills and expertise. Cross-training staff members can also provide flexibility in handling various roles during busy periods. Regular Performance Reviews: Conduct regular reviews of your practice’s performance to identify areas for improvement. Use key performance indicators (KPIs) to measure efficiency, patient satisfaction, and other important metrics. Optimizing your practice workflow and scheduling not only improves the operational efficiency of your practice but also enhances patient satisfaction by minimizing wait times and providing a more organized and pleasant experience. At HS MED Solutions, our practice management tools are designed to help you streamline your operations and make the most of your resources, ensuring a well-run and patient-centric practice. Focus on Staff Training and Development Continuous staff training and professional development are vital components of effective practice management. Investing in your staff’s education ensures they stay updated with the latest industry practices and technologies, leading to improved efficiency, better patient care, and enhanced job satisfaction. Here are some key reasons to focus on staff training and development: Improved Skills and Knowledge: Regular training helps staff members stay current with the latest medical billing codes, compliance regulations, and healthcare technologies, ensuring they can perform their tasks accurately and efficiently. Enhanced Patient Care: Well-trained staff are better equipped to handle patient interactions, provide accurate information, and deliver high-quality care. Increased Efficiency: Continuous professional development can help staff learn new skills and techniques to streamline workflows and reduce administrative burdens. Higher Job Satisfaction: Providing opportunities for growth and development can lead to higher job satisfaction and employee retention, reducing turnover rates in your practice. Actionable Tip: Examples of Training Programs and Resources Online Courses and Webinars: Numerous online platforms offer courses and webinars on medical billing, practice management, and healthcare technologies. Websites like Coursera, Udemy, and LinkedIn Learning provide access to a wide range of relevant topics. Professional Certifications: Encourage staff to pursue certifications such as Certified Professional Coder (CPC), Certified Medical Reimbursement Specialist (CMRS), or Certified Medical Manager (CMM). These credentials demonstrate expertise and commitment to professional development.
Urgent Care Centers and Emergency Clinics

Providing Exceptional Urgent Care Services Top-Quality Urgent Care Services At HS Med Solutions, we understand that your health is of the utmost importance. That’s why we proudly deliver top-quality urgent care services, focusing on exceptional patient care.Whether you need treatment for a minor injury or illness, or you require more comprehensive care, our team of experienced healthcare providers is here to help. Schedule an Appointment Now Introduction to Urgent Care and Emergency Clinics Urgent care centers and emergency walk-in clinics have become indispensable parts of the healthcare system, providing essential services that ensure patients receive prompt medical attention when needed. These facilities are specifically designed to handle non-life-threatening conditions, offering a critical alternative to both primary care and emergency rooms. By understanding the distinctions and benefits of urgent care centers and emergency walk-in clinics, patients can make informed decisions about where to seek care. What Are Urgent Care Centers and Emergency Walk-In Clinics? Urgent care centers are medical facilities equipped to treat various minor injuries and illnesses that require immediate attention but are not severe enough to necessitate a visit to an emergency room. Typical services include treatment for sprains, fractures, cuts requiring stitches, infections, and routine vaccinations. These centers often operate beyond regular office hours, including evenings and weekends, providing a convenient option for immediate care when primary care offices are closed. Emergency walk-in clinics, while similar to urgent care centers, are often better equipped to handle more severe conditions that still do not reach the threshold of emergency room care. These clinics might offer advanced diagnostic services like imaging and lab tests on-site, enabling comprehensive care for conditions that require prompt but not critical intervention. Differences Between Urgent Care, Emergency Care, and Primary Care Understanding the differences between urgent care, emergency care, and primary care is crucial for both patients and healthcare providers. Urgent Care: These centers provide immediate attention for non-emergency conditions. They are ideal for issues like minor fractures, sprains, infections, and minor cuts. Urgent care centers are designed to offer quick and efficient care, often without the need for an appointment. Emergency Care: Emergency rooms are equipped to handle life-threatening conditions and serious injuries. Situations such as severe chest pain, difficulty breathing, major trauma, and significant bleeding require the comprehensive resources available in an emergency room. Emergency care is critical for conditions that pose an immediate risk to life or long-term health. Primary Care: Primary care providers manage overall health and wellness, offering preventive care, routine check-ups, and management of chronic conditions. They serve as the first point of contact for health concerns and coordinate care with specialists as needed. Primary care is essential for maintaining long-term health and managing ongoing health issues. Urgent care centers and emergency walk-in clinics play a pivotal role in the healthcare ecosystem, offering accessible, immediate care for conditions that are urgent but not life-threatening. This ensures that patients receive the right level of care when they need it most, while also reducing the strain on emergency rooms and enhancing overall healthcare efficiency. Availability and Accessibility The Growing Demand for Immediate Medical Attention The increasing demand for “urgent care open now” and “24-hour urgent care clinics near me” reflects the public’s growing need for immediate medical attention outside of regular office hours. These search trends highlight how urgent care centers have become a crucial component in the healthcare landscape, providing accessible and timely care when primary care services are unavailable. Bridging the Gap Between Primary Care and Emergency Rooms Urgent care centers are designed to bridge the gap between primary care and emergency rooms, offering a convenient alternative for patients who need prompt attention but do not require the extensive resources of an emergency room. These centers are typically open evenings and weekends, ensuring that medical care is available beyond the traditional 9-to-5 schedule. This extended availability is particularly beneficial for individuals with busy lifestyles or those who experience sudden health issues outside of regular office hours. Extended Hours for Busy Lifestyles Moreover, urgent care centers are strategically located to serve local communities, making it easier for patients to find immediate care close to home. By providing walk-in services without the need for an appointment, these centers offer a flexible and accessible option for non-emergency situations, reducing the need for patients to endure long waits in emergency rooms or delay care until primary care offices reopen. Strategic Locations for Community Access The accessibility of urgent care centers also alleviates the burden on emergency departments, allowing them to focus on treating life-threatening conditions. This not only improves the efficiency of emergency rooms but also ensures that patients receive the appropriate level of care for their medical needs. Urgent care centers can handle a variety of issues, including minor injuries, infections, fractures, and routine vaccinations, providing comprehensive care in a timely manner. Enhancing Healthcare Accessibility and Efficiency By filling the gap when primary care is unavailable, urgent care centers enhance the overall accessibility and efficiency of the healthcare system. They offer a critical service that meets the immediate needs of patients, ensuring that quality medical care is always within reach, regardless of the time of day. Services Offered at Urgent Care Centers Urgent care centers are equipped to provide a wide range of medical services, ensuring that patients receive prompt and effective treatment for various health concerns. These facilities are designed to handle both common and specialized medical needs, offering a comprehensive solution for immediate care. Common Services Provided Urgent care centers offer numerous services that address a variety of minor health issues, making them an ideal choice for non-emergency situations. Some of the most common services include: Minor Injuries: Treatment for sprains, strains, minor fractures, cuts, and bruises. Urgent care centers can provide stitches, splints, and other necessary interventions to address these injuries promptly. Infections: Diagnosis and treatment of common infections such as respiratory infections, ear infections, urinary tract infections, and skin infections. Quick access to care helps prevent the progression of these conditions. Vaccinations: Routine immunizations, including flu shots,
The Evolution from Old to New Medical Billing Systems
Medical billing systems have undergone substantial transformations in the continuously evolving healthcare landscape. The shift from manual processes and paper-based records to automated systems and Electronic Health Records (EHRs) has revolutionized the way healthcare providers manage billing and revenue cycles. These changes not only enhance efficiency and accuracy but also improve transparency and patient experience. In this article, we will explore the key differences between old and new medical billing systems, highlighting the benefits of modern healthcare billing technology and the impact on financial performance for healthcare providers. Importance The modernization of medical billing systems is not just a technological upgrade; it’s a crucial step toward improving the overall healthcare delivery process. With the healthcare industry facing increasing demands for efficiency, accuracy, and cost-effectiveness, the shift from manual processes to automated systems and Electronic Health Records (EHRs) is essential. This transformation ensures faster payment cycles, reduces the likelihood of errors, and enhances regulatory compliance. Additionally, improved transparency and patient experience are pivotal in building trust and satisfaction among patients. In this article, we delve into the significance of adopting new medical billing systems, the challenges of the old methods, and the remarkable benefits that modern technology brings to healthcare providers and patients alike. The Old Medical Billing System The traditional medical billing system reckoned heavily on homemade processes and paper- grounded records, which posed significant challenges for healthcare providers. This antiquated approach involved a series of labor- ferocious tasks, from filling out paper forms to manually entering data into separate systems. The reliance on physical documents not only increased the liability of crimes but also made the entire billing process clumsy and time- consuming. Key Characteristics: Paper-Based Records: Patient information, billing details, and medical histories were documented on paper, requiring meticulous filing and storage. This system was prone to misplacements and damage, leading to potential data loss. Manual Data Entry: Healthcare staff had to manually enter data into billing systems, which was a slow and error-prone process. Any mistakes could result in claim denials or delays, impacting the financial performance of healthcare providers. Fragmented Systems: Different aspects of patient management and billing were handled by separate systems, creating inefficiencies and communication gaps. Coordinating information between departments was challenging, often leading to inconsistencies. Delayed Payments: The manual nature of old medical billing systems meant that processing times were lengthy, causing delays in payments from insurance companies. This could strain the cash flow of healthcare practices. Limited Transparency: Tracking the status of claims and payments was difficult, with limited visibility for both providers and patients. This lack of transparency could lead to confusion and dissatisfaction among patients. Regulatory Challenges: Ensuring compliance with healthcare regulations and standards was more complex with manual systems. Keeping up with changes in codes and requirements added to the administrative burden. Despite these challenges, many healthcare providers continued to use old medical billing systems due to familiarity and resistance to change. However, the inefficiencies and risks associated with these outdated methods highlighted the need for a more streamlined and effective solution. The New Medical Billing System The advent of new medical billing systems has revolutionized the healthcare industry by addressing the inefficiencies and challenges of traditional methods. Leveraging advancements in technology, these modern systems offer a range of benefits that enhance accuracy, efficiency, and transparency in the billing process. Key Characteristics: Electronic Health Records (EHRs): Modern medical billing systems integrate with EHRs, allowing for seamless access to patient records and billing information. This integration reduces the need for redundant data entry and minimizes errors. Automated Processes: Automation plays a critical role in new billing systems. From automatic claim submissions to real-time eligibility verification, automation speeds up processes and reduces manual workloads, leading to quicker reimbursements. Real-Time Processing: Electronic claims submission allows for real-time processing, significantly reducing the turnaround time for payments. This improvement in the payment cycle enhances cash flow for healthcare providers. Enhanced Transparency: Modern systems provide tools that allow both providers and patients to track the status of claims and payments. This transparency helps in maintaining trust and ensures patients are better informed about their billing details. Integrated Systems: New medical billing systems are often part of integrated healthcare management software suites. This integration ensures that all aspects of patient care and administration are connected, reducing inefficiencies and communication gaps. Regulatory Compliance: Compliance with regulations such as HIPAA and ICD-10 is easier with modern systems. These systems are designed to stay up-to-date with regulatory changes, ensuring that healthcare providers meet all legal requirements. Data Analytics: Advanced analytics capabilities allow healthcare providers to analyze billing data, identify trends, and optimize financial performance. This data-driven approach helps in making informed decisions and improving overall operations. Patient Portals: Modern billing systems often include patient portals that allow patients to view their billing information, make payments online, and communicate with healthcare providers. This enhances the patient experience by providing easy access to important information. Benefits: Efficiency and Accuracy: Automation and integration reduce errors and streamline processes, resulting in more accurate billing and quicker reimbursements. Financial Performance: Improved cash flow and reduced administrative costs contribute to better financial health for healthcare providers. Patient Experience: Enhanced transparency and easy access to billing information improve patient satisfaction and trust. Challenges: Implementation Costs: Upgrading to a new system can involve significant upfront costs and require a substantial investment in technology and training. Training and Adaptation: Healthcare staff need to be trained to use new systems effectively. This transition period can be challenging and may temporarily disrupt operations. Data Security: Ensuring the security of electronic data is paramount. Modern systems must have robust security measures to protect sensitive patient information. Conclusion The shift from old to new medical billing systems represents a significant advancement in the healthcare assiduity. By embracing ultramodern technology, healthcare providers can achieve lesser effectiveness, delicacy, and patient satisfaction, eventually leading to better fiscal and functional performance. Why Modern Medical Billing Systems Are Essential for Doctors At HS Med Solutions, we understand the critical role that efficient and accurate medical
Why Medical Billing Companies Are Essential for Doctors

Introduction: In the modern healthcare landscape, the complexities of medical billing can be overwhelming for doctors. Engaging a specialized medical billing company is not just a convenience but a necessity for healthcare providers who wish to focus on patient care. This article will explore the key reasons why medical billing companies are indispensable for doctors. Expertise and Accuracy: Medical billing companies employ professionals who are well-versed in the intricacies of billing codes, insurance policies, and regulatory requirements. Their expertise ensures that claims are processed accurately, minimizing errors and delays. Time Management: Doctors can save a significant amount of time by outsourcing billing tasks. This allows them to devote more time to patient care and other critical aspects of their practice, rather than getting bogged down with administrative duties. Financial Benefits: Outsourcing billing to a professional company can lead to higher reimbursement rates and faster payments. Medical billing companies skillfully optimize claims and reduce the chances of denials, ultimately enhancing the financial health of a practice. Compliance and Risk Management: Medical billing companies stay up-to-date with ever-changing healthcare regulations and compliance requirements. By ensuring adherence to these standards, they help doctors avoid potential legal issues and penalties. Enhanced Patient Satisfaction: When billing processes are smooth and efficient, it positively impacts the overall patient experience. Patients appreciate clear, accurate billing and the ability to resolve any issues promptly, contributing to their satisfaction and trust in the practice. Conclusion: For doctors looking to streamline their operations, improve financial performance, and focus on providing excellent patient care, partnering with a medical billing company is a strategic move. The benefits of expertise, time management, financial gains, compliance, and patient satisfaction make these companies an essential part of modern medical practices. HS Med Solutions: Your Trusted Partner At HS Med Solutions, we understand the challenges that come with managing medical billing. Our experienced professionals dedicate themselves to providing accurate, efficient, and compliant billing services tailored to your practice’s unique needs. Let us handle the complexities of medical billing so you can concentrate on what you do best—caring for your patients. Contact us today to learn how we can support your practice.
Understanding the Basics of Medical Insurance Billing

Introduction A Brief Introduction to Medical Insurance Billing Medical insurance billing is a crucial aspect of the healthcare industry, involving the process of submitting and following up on claims with health insurance companies to receive payment for services provided by healthcare providers. This complex procedure ensures that healthcare providers are compensated for their services, while patients are billed accurately according to their insurance policies. Importance of Understanding the Basics Understanding the basics of medical insurance billing is essential for several reasons. For patients, it helps in comprehending their healthcare expenses, navigating their insurance coverage, and avoiding unexpected bills. For medical professionals and billing specialists, it ensures accurate and efficient billing processes, reduces claim denials, and improves overall patient satisfaction. Knowledge of medical billing also aids in compliance with regulations, preventing legal issues and financial losses. Who This Article is For This article is designed for a diverse audience, including patients seeking to understand their medical bills, medical professionals involved in the billing process, and billing specialists aiming to enhance their expertise. Whether you are new to the field or looking to refresh your knowledge, this guide will provide valuable insights into the fundamentals of medical insurance billing. What is Medical Insurance Billing? Definition and Overview Medical insurance billing is the process through which healthcare providers submit claims to insurance companies to receive payment for services rendered to patients. This process involves a detailed and systematic approach to ensure that healthcare providers are reimbursed for their services and that patients are billed correctly according to their insurance policies. The medical billing process begins when a patient receives a service from a healthcare provider. The provider documents the service using specific medical codes, which are then used to create a bill or claim. This claim is submitted to the patient’s insurance company, which reviews the claim and determines the amount to be paid based on the patient’s insurance policy. The remaining balance, if any, is billed to the patient. The Role of Medical Insurance Billing in Healthcare Medical insurance billing plays a pivotal role in the healthcare industry for several reasons: Ensuring Financial Stability: Accurate medical billing ensures that healthcare providers are compensated for their services, which is essential for maintaining the financial health of medical practices, hospitals, and clinics. Without proper billing, providers would face financial difficulties, potentially affecting the quality of care they can offer. Streamlining the Payment Process: Medical billing creates a streamlined process for managing and processing payments. It ensures that claims are submitted promptly and accurately, reducing delays in payment and improving cash flow for healthcare providers. Enhancing Patient Experience: When medical billing is handled efficiently, patients receive clear and accurate bills, reducing confusion and frustration. Understanding their bills helps patients manage their healthcare expenses better and prevents unexpected charges. Compliance and Legal Protection: Proper medical billing ensures compliance with various regulations and standards, such as the Health Insurance Portability and Accountability Act (HIPAA). Compliance protects healthcare providers from legal issues and financial penalties. Data Collection and Analysis: The medical billing process generates a wealth of data that can be analyzed to identify trends, optimize billing practices, and improve overall efficiency. This data is valuable for making informed decisions and enhancing the quality of care. In summary, medical insurance billing is a critical component of the healthcare system, ensuring that providers are paid for their services, patients understand their financial responsibilities, and the entire payment process is efficient and compliant with regulations. Key Terminology Understanding the terminology used in medical insurance billing is crucial for navigating the billing process effectively. Here are some common terms explained in simple language: Premium A premium is the amount of money that an individual or employer pays to an insurance company regularly (usually monthly) to maintain health insurance coverage. Think of it as a membership fee for having insurance. Deductible A deductible is the amount of money a patient must pay out-of-pocket for healthcare services before the insurance company starts to pay its share. For example, if your deductible is $1,000, you must pay that amount before your insurance begins covering costs. Co-payment (Co-pay) A co-payment is a fixed amount that a patient pays for a specific healthcare service, such as a doctor’s visit or prescription medication, at the time of service. For instance, you might pay $20 for a doctor’s appointment, while your insurance covers the rest. Co-insurance Co-insurance is the percentage of the cost of a healthcare service that a patient must pay after meeting their deductible. For example, if your insurance covers 80% of a service, you would pay the remaining 20%. Explanation of Benefits (EOB) An Explanation of Benefits (EOB) is a statement provided by the insurance company after a claim has been processed. It details what services were covered, how much the insurance paid, and what portion of the costs the patient is responsible for. It is not a bill but an informational document. Out-of-Pocket Maximum The out-of-pocket maximum is the maximum amount a patient has to pay for covered services in a plan year. After reaching this limit, the insurance company pays 100% of the costs for covered services. This includes deductibles, co-payments, and co-insurance. In-Network vs. Out-of-Network In-network refers to healthcare providers and facilities that have a contract with your insurance company to provide services at a negotiated rate. Out-of-network providers do not have such contracts, and using them typically results in higher costs for the patient. Claim A claim is a formal request for payment submitted to the insurance company by the healthcare provider or the patient after receiving services. The claim details the services provided and the associated costs. Pre-authorization Pre-authorization (or prior authorization) is approval from the insurance company that may be required before certain services or medications are covered. This ensures that the service or medication is deemed medically necessary. Network A network is a group of doctors, hospitals, and other healthcare providers that have agreed to provide medical care at negotiated rates for members of a specific insurance
Trends in Medical Billing
As the healthcare landscape continues to evolve, so does the intricate web of medical billing and coding. From technological advancements to regulatory changes, the field of medical billing is witnessing a significant transformation. In this article, we delve into the latest trends shaping the realm of medical billing, exploring how these trends are revolutionizing processes, improving efficiency, and ensuring compliance within the healthcare industry. Join us on a journey through the dynamic world of medical billing as we uncover the key trends driving innovation and change in this vital aspect of healthcare administration. Telemedicine Telemedicine has emerged as a game-changer in the healthcare landscape, offering remote access to medical services and consultations. With the rise of telemedicine comes the need for specialized billing practices tailored to this digital frontier. e-medicine billing encompasses the processes and procedures involved in billing for medical services delivered remotely, utilizing telecommunications technology. Telemedicine Billing: Telemedicine billing involves coding and billing for virtual healthcare services, such as teleconsultations, remote monitoring, and telehealth visits. Providers must adhere to specific guidelines and codes established by insurance payers and regulatory bodies to accurately bill for telemedicine encounters. This includes documenting patient information, service codes, and modifiers to ensure proper reimbursement. Value-Based Care As the healthcare industry continues to evolve, so do the methodologies and practices surrounding medical billing. One of the most significant trends influencing this field is the shift towards value-based care. This paradigm shift emphasizes delivering high-quality care and improved patient outcomes while controlling costs. In this article, we delve into the intricacies of value-based care, exploring its impact on medical billing and the implications for healthcare providers and patients. Redefining Medical Billing: Value-based care represents a transformative approach to healthcare delivery and reimbursement, focusing on the quality and effectiveness of care rather than the volume of services provided. This model aims to enhance patient outcomes and reduce healthcare costs by incentivizing providers to deliver efficient, high-quality care. Key Components of Value-Based Care: Quality Metrics: Providers are assessed based on specific quality metrics, including patient outcomes, readmission rates, and patient satisfaction scores. These metrics ensure that care is patient-centered and effective, guiding reimbursement decisions and fostering continuous improvement in care quality. Reimbursement Models: Value-based care introduces various reimbursement models such as bundled payments, shared savings programs, and accountable care organizations (ACOs). These models incentivize providers to deliver cost-effective, high-quality care, aligning financial rewards with patient health outcomes. Care Coordination: Effective care coordination is essential in value-based care. Providers must collaborate across specialties and care settings to ensure seamless patient care, preventing unnecessary treatments or hospitalizations and improving overall care efficiency. Patient Engagement: Engaging patients in their own care is a cornerstone of value-based care. This involves educating patients about their conditions and treatment options, encouraging adherence to care plans, and promoting preventive care to improve health outcomes and patient satisfaction. Benefits of Value-Based Care: Improved Patient Outcomes: By focusing on quality and outcomes, value-based care enhances patient health and reduces complications, leading to better overall health outcomes and higher patient satisfaction. Cost Reduction: Value-based care reduces healthcare costs by eliminating unnecessary procedures and hospital readmissions and emphasizing preventive care. This cost-efficiency benefits both patients and the healthcare system. Enhanced Provider Accountability: Providers are held accountable for the quality and efficiency of the care they deliver. This accountability fosters a culture of continuous improvement, ensuring that healthcare services are patient-centered and effective. Challenges and Considerations: Implementing value-based care poses several challenges. Transitioning from traditional fee-for-service models requires significant changes in billing practices and financial structures. Aligning incentives across various stakeholders, ensuring accurate measurement of quality metrics, and investing in data analytics and health IT systems are critical to supporting value-based care initiatives. Additionally, providers must navigate regulatory requirements and adapt to evolving reimbursement policies. In conclusion, the shift towards value-based care is a pivotal trend in medical billing, transforming how healthcare providers deliver and bill for services. By embracing value-based care principles, providers can enhance patient outcomes, reduce costs, and navigate the complex healthcare landscape more effectively. Understanding and adapting to this trend is essential for healthcare providers aiming to deliver high-quality, patient-centered care in the modern healthcare environment. Automation and Artificial Intelligence The healthcare industry is undergoing a significant transformation, driven by technological advancements that are reshaping various aspects of medical practice. One of the most notable trends in medical billing is the integration of automation and artificial intelligence (AI). These technologies are revolutionizing the billing process, enhancing efficiency, accuracy, and overall healthcare delivery. In this article, we explore the impact of automation and AI on medical billing, highlighting their benefits and implications for healthcare providers and patients. Revolutionizing Medical Billing: Automation and AI are at the forefront of innovation in medical billing, streamlining processes, reducing errors, and improving financial outcomes for healthcare providers. These technologies are designed to handle repetitive tasks, analyze vast amounts of data, and make intelligent decisions, transforming how billing operations are conducted. Key Components of Automation and AI in Medical Billing: Automated Data Entry and Processing: Automation significantly reduces the manual effort involved in data entry and processing. By leveraging AI-driven software, healthcare providers can automatically capture, verify, and process patient information, claims, and billing codes. This not only speeds up the billing cycle but also minimizes human errors, ensuring more accurate billing. Claim Scrubbing and Error Reduction: AI-powered claim scrubbing tools can identify and correct errors in billing codes before claims are submitted to payers. These tools analyze claims for potential issues, such as coding inaccuracies or missing information, reducing the likelihood of claim denials and ensuring faster reimbursement. Predictive Analytics: AI algorithms can analyze historical billing data to predict trends and identify patterns. This predictive capability helps healthcare providers optimize billing practices, forecast revenue, and identify potential issues before they impact the bottom line. For instance, AI can flag claims that are likely to be denied, allowing proactive measures to be taken. Revenue Cycle Management: Automation and AI streamline the entire revenue cycle, from patient registration to final payment.
Revenue Cycle Management
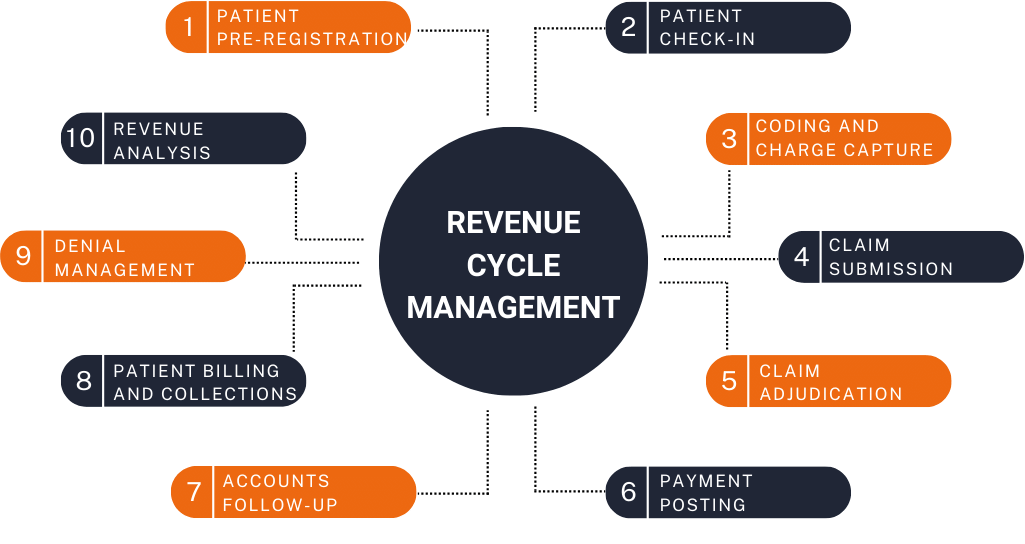
Revenue Cycle Management Revenue Cycle Management (RCM) is a crucial financial process used by healthcare organizations to manage the administrative and clinical functions associated with patient service revenue. It encompasses the entire lifecycle of a patient’s account, from initial scheduling and registration to the final payment of the balance. The primary goal of RCM is to optimize the financial performance of healthcare providers by ensuring timely and accurate billing, maximizing revenue, and reducing the costs associated with managing patient accounts. Here are the key components of Revenue Cycle Management: Patient Scheduling and Registration Insurance Verification and Authorization Patient Encounter and Documentation Charge Capture Coding Claim Submission Payment Posting Denial Management Patient Billing and Collections Reporting and Analysis Patient Scheduling and Registration: Efficient patient scheduling and registration are foundational elements of effective Revenue Cycle Management (RCM) in healthcare. These initial steps not only set the tone for a patient’s experience but also significantly impact the financial health of medical practices. Here’s how optimizing these processes can enhance overall RCM. The Importance of Patient Scheduling in RCM Patient scheduling is the first point of contact between a patient and a healthcare provider. Proper scheduling ensures that healthcare resources are utilized efficiently, reducing wait times and improving patient satisfaction. Here’s why it’s vital: Optimizing Resource Utilization: Effective scheduling maximizes the use of medical staff and facilities, ensuring that no resources are underused or overburdened. This balance is crucial for maintaining operational efficiency and controlling costs. Reducing No-Shows and Cancellations: Implementing automated reminders and easy rescheduling options can significantly reduce the rate of no-shows and last-minute cancellations, which are costly to the practice. Enhancing Patient Experience: Streamlined scheduling processes contribute to a positive patient experience by minimizing wait times and ensuring timely care, which can improve patient retention and satisfaction. Streamlined Registration: The Gateway to Accurate Billing Patient registration is more than just collecting information; it’s about ensuring the accuracy and completeness of patient data to facilitate smooth billing and claims processing. Here’s how a streamlined registration process supports RCM: Accurate Information Collection: Collecting comprehensive and accurate patient information during registration helps prevent billing errors. This includes personal details, medical history, and, crucially, insurance information. Insurance Verification and Pre-Authorization: Verifying insurance coverage and obtaining necessary pre-authorizations during registration can prevent claim denials and delays in reimbursement, which are critical for maintaining cash flow. Efficiency in Data Handling: Utilizing electronic health records (EHRs) and integrated systems ensures that patient data is readily accessible and correctly recorded, reducing the risk of errors and improving the overall efficiency of the RCM process. Best Practices for Enhancing Scheduling and Registration in RCM To optimize patient scheduling and registration within the context of Revenue Cycle Management, consider the following best practices: Implement Advanced Scheduling Software: Use scheduling software that offers automated reminders, online booking options, and integrates with EHR systems to streamline the scheduling process and reduce administrative burden. Train Staff Thoroughly: Ensure that all staff involved in scheduling and registration are well-trained in the use of the systems and understand the importance of accurate data collection and insurance verification. Utilize Patient Portals: Encourage patients to use online portals to update their information, schedule appointments, and complete pre-registration forms. This not only saves time but also reduces the risk of errors. Regularly Review and Update Processes: Continually assess the scheduling and registration processes to identify areas for improvement. Implement feedback from patients and staff to enhance the overall experience and efficiency. Integrate RCM and Clinical Systems: Ensure that your RCM systems are integrated with clinical management systems to facilitate seamless data flow and enhance the accuracy of patient records, which is crucial for effective billing and claims management. Conclusion Patient scheduling and registration are critical steps in the Revenue Cycle Management process that can significantly influence a healthcare organization’s financial performance. By optimizing these processes, healthcare providers can improve resource utilization, enhance patient satisfaction, and ensure accurate billing and timely reimbursement. Implementing advanced systems, training staff, and regularly updating processes are key strategies for achieving these goals. In the dynamic landscape of healthcare, efficient scheduling and registration are not just operational necessities—they are strategic imperatives for financial sustainability and growth. Insurance Verification and Authorization Insurance verification and authorization are critical components of Revenue Cycle Management (RCM) that directly impact a healthcare organization’s financial health. By ensuring that services are covered and authorized before they are rendered, healthcare providers can minimize claim denials, reduce financial risks, and enhance patient satisfaction. Here’s a closer look at how these processes can be optimized within the framework of RCM. The Role of Insurance Verification in RCM Insurance verification involves confirming a patient’s insurance coverage, benefits, and eligibility for services before the appointment or procedure. This step is crucial for several reasons: Preventing Claim Denials: By verifying insurance information upfront, providers can avoid the common pitfall of claim denials due to ineligible services or lapsed coverage. This proactive approach ensures that the services rendered are reimbursable. Clarifying Patient Financial Responsibility: Accurate insurance verification helps clarify what portion of the cost is covered by insurance and what the patient will need to pay out-of-pocket. This transparency improves patient satisfaction and reduces the likelihood of unpaid bills. Streamlining the Billing Process: Verifying insurance details before service delivery streamlines the billing process, reducing administrative burdens and improving the efficiency of claims submission. The Importance of Authorization in RCM Authorization, or prior authorization, is the process of obtaining approval from an insurance company before providing certain medical services. This step is essential for: Ensuring Reimbursement: Many insurance plans require prior authorization for specific procedures or treatments. Obtaining this approval is crucial for ensuring that the provider will be reimbursed for these services. Reducing Financial Risk: Without prior authorization, providers risk performing services that might not be covered, leading to significant financial losses. Ensuring authorization beforehand mitigates this risk. Compliance with Insurance Policies: Adhering to the authorization requirements of insurance companies helps maintain compliance and avoid potential legal and financial penalties. Best Practices for Insurance Verification and Authorization
Revealing MedSolutions: Unlocking the Secrets to Billing Efficiency

Revealing MedSolutions: Unlocking the Secrets to Billing Efficiency Demystifying MedSolutions Inc: Unlocking the Secrets of Billing Efficiency Welcome to MedSolutions Inc, where efficiency and billing secrets are demystified. In this article, we delve into the intricate world of medical billing to uncover the strategies employed by MedSolutions Inc that have revolutionized the industry. With a keen focus on precision and optimization, MedSolutions Inc has emerged as a leading player in the field of medical billing. Their commitment to streamlining the billing process and improving reimbursement rates has allowed healthcare providers to maximize their revenue and minimize administrative burdens. At MedSolutions Inc, we understand that accurate and efficient billing is the lifeblood of any healthcare organization. Through advanced technology and a dedicated team of experts, they have developed a seamless billing system that minimizes errors and ensures timely reimbursement. Join us on this journey as we explore the inner workings of MedSolutions Inc and uncover the secrets behind their billing efficiency. Whether you are a healthcare professional looking to enhance your revenue cycle management or a patient curious about the behind-the-scenes process, this article will provide valuable insights into the world of medical billing like never before. Understanding the importance of billing efficiency in healthcare Efficient medical billing is crucial for the financial health of healthcare organizations. It ensures that healthcare providers receive timely payments for services rendered, allowing them to continue providing quality care to patients. However, the billing process can be complex and prone to errors, leading to delays in reimbursement and lost revenue. At MedSolutions Inc, the importance of billing efficiency is ingrained in their core values. They understand that accurate and efficient billing is the lifeblood of any healthcare organization. By streamlining the billing process, healthcare providers can focus on patient care without worrying about administrative burdens. Common challenges in medical billing Medical billing is a complex process that involves numerous stakeholders, including healthcare providers, insurance companies, and patients. With so many parties involved, challenges are bound to arise. Some common challenges in medical billing include: 1. Coding Errors: Incorrect coding can lead to claim denials and delayed payments. Medical coders must accurately translate diagnoses and procedures into standardized codes to ensure proper reimbursement. 2. Insurance Verification: Verifying patient insurance coverage can be time-consuming and prone to errors. Failure to verify insurance coverage upfront can result in denied claims and delayed payments. 3. Claim Denials: Insurance companies often deny claims for various reasons, such as missing information or lack of medical necessity. Resubmitting denied claims can be time-consuming and impact cash flow. 4. Payment Delays: Insurance companies may take weeks or even months to process claims and issue payments. These delays can disrupt cash flow and hinder the financial stability of healthcare organizations. Key components of an efficient billing process To achieve billing efficiency, healthcare organizations must have a well-defined process in place. The key components of an efficient billing process include: 1. Accurate Documentation: Accurate and detailed documentation of patient encounters is essential for proper billing. Healthcare providers should ensure that all services rendered are clearly documented to support their claims. 2. Timely Claims Submission: Submitting claims promptly is crucial to avoid payment delays. Claims should be submitted within the designated timeframe to ensure timely reimbursement. 3. Effective Coding: Proper coding is the foundation of accurate billing. Medical coders should stay up to date with the latest coding guidelines and ensure that diagnoses and procedures are coded correctly. 4. Insurance Verification: Verifying patient insurance coverage before providing services helps avoid claim denials. It is important to confirm eligibility, coverage limits, and any pre-authorization requirements. 5. Robust Billing Software: Utilizing advanced billing software can streamline the entire billing process. The software should have features such as automated claim submission, real-time eligibility verification, and denial management. Implementing technology for streamlined billing operations Technology plays a critical role in streamlining billing operations and improving efficiency. MedSolutions Inc leverages advanced technology to optimize the billing process. Here are some ways technology can enhance billing efficiency: 1. Electronic Health Records (EHR): EHR systems allow for seamless integration of patient information, reducing the risk of errors and duplicate data entry. This integration enables accurate and efficient billing. 2. Automated Claim Submission: Manual claim submission is time-consuming and prone to errors. Automated claim submission streamlines the process, ensuring timely submission and reducing the risk of denials. 3. Real-time Eligibility Verification: Technology can provide instant access to insurance eligibility information, allowing healthcare providers to verify coverage and avoid claim denials. 4. Analytics and Reporting: Advanced billing software can generate detailed reports and analytics, providing insights into the financial health of a healthcare organization. These reports help identify areas for improvement and maximize revenue. Best practices for enhancing billing efficiency In addition to implementing technology, there are several best practices that healthcare organizations can adopt to enhance billing efficiency. Here are some key best practices: 1. Regular Staff Training: Keeping staff up to date with the latest coding guidelines and billing regulations is crucial. Regular training sessions ensure that employees are equipped with the knowledge and skills to handle billing efficiently. 2. Streamlined Documentation Process: Streamlining the documentation process reduces errors and ensures accurate billing. Standardizing documentation templates and implementing electronic documentation systems can improve efficiency. 3. Claims Scrubbing: Conducting thorough claims scrubbing before submission helps identify potential errors or missing information. This proactive approach reduces the risk of claim denials and ensures clean claims are submitted. 4. Denial Management: Developing a robust denial management process is essential. Healthcare organizations should have dedicated staff to investigate claim denials, resubmit claims when appropriate, and identify areas for improvement. 5. Regular Audits: Conducting regular internal audits helps identify billing errors and areas for improvement. Audits can also ensure compliance with regulations and identify any potential fraudulent activities. By adopting these best practices, healthcare organizations can optimize their billing processes and improve reimbursement rates. Case study: How MedSolutions Inc transformed its billing process MedSolutions Inc has successfully transformed its billing process, setting an industry standard for efficiency.
Medical Billing Software Comparison

Medical Billing Software Comparison In the fast-paced world of healthcare, efficiency and accuracy are paramount. Medical billing software plays a crucial role in streamlining revenue cycle management for healthcare providers, ensuring that claims processing, compliance, and financial performance are optimized. In this comprehensive guide, we delve into the realm of medical billing software, exploring its types, key features, benefits, and the essential factors to consider when choosing the right solution for your practice. Introduction to Medical Billing Software Medical billing software is a digital solution designed to automate and manage the billing process in healthcare facilities. It integrates seamlessly with practice management systems and electronic health records (EHR), offering a centralized platform for billing, coding, claims processing, and revenue cycle management. Types of Medical Billing Software There are several types of medical billing software available, catering to the diverse needs of healthcare providers. Some common types include: 1 – Stand-Alone Billing Software: Focus: These solutions are designed specifically for billing and claims processing. Suitability: Ideal for small to mid-sized practices that primarily require billing functionality without extensive practice management features. Features: Stand-alone billing software typically includes claim generation, submission, and tracking, as well as coding assistance and basic reporting capabilities. Benefits: Simplifies billing processes, reduces errors, and streamlines reimbursement workflows. 2 – Integrated Practice Management Systems (PMS): Focus: PMS platforms encompass a broader range of functionalities beyond billing, including scheduling, patient management, and reporting. Suitability: Suitable for practices looking for a comprehensive solution that integrates billing with other practice management tasks. Features: In addition to billing features, PMS software offers appointment scheduling, patient demographics management, revenue cycle analytics, and financial reporting. Benefits: Centralizes practice operations, improves workflow efficiency, enhances patient experience, and provides holistic insights into practice performance. 3 – EHR-Integrated Billing Software: Focus: These solutions combine electronic health record (EHR) capabilities with billing functionalities. Suitability: Ideal for practices seeking seamless integration between clinical data and billing processes, eliminating duplicate data entry and improving accuracy. Features: EHR-integrated billing software includes EHR functionality such as patient charting, clinical documentation, e-prescribing, alongside billing features like claim submission, coding assistance, and revenue cycle management. Benefits: Streamlines clinical and administrative workflows, improves care coordination, enhances billing accuracy, and supports meaningful use of EHR technology. 4 – Cloud-Based Billing Software: Focus: Cloud-based solutions host billing software on remote servers accessible via the internet, offering flexibility and scalability. Suitability: Suitable for practices of all sizes looking for a cost-effective, scalable, and accessible billing solution. Features: Cloud-based billing software provides remote access, automatic updates, data backup, and integration with other cloud services. Benefits: Enables anytime, anywhere access to billing data, reduces IT infrastructure costs, improves data security, and facilitates collaboration among remote teams. 5 – Specialty-Specific Billing Software: Focus: These solutions are tailored to meet the unique billing and coding requirements of specific medical specialties, such as cardiology, dermatology, or mental health. Suitability: Ideal for practices with specialized billing needs and complex reimbursement scenarios. Features: Specialty-specific billing software includes specialty-specific code sets, billing rules, documentation templates, and reporting capabilities tailored to the specialty’s billing nuances. Benefits: Optimizes billing accuracy, reduces claim denials, ensures compliance with specialty-specific coding guidelines, and maximizes reimbursement for specialized services. By understanding the different types of medical billing software and their respective features, healthcare providers can choose a solution that aligns with their practice’s size, specialty, workflow preferences, and long-term strategic goals. Key Features to Look For When evaluating medical billing software, it’s essential to consider the following key features: 1 – Claims Submission and Tracking: Electronic Claim Submission: Ensure the software supports electronic claim submission to insurance companies, Medicare, and Medicaid, speeding up reimbursement processes. Claim Tracking: A robust system for tracking claims status is crucial, allowing you to identify and address any issues promptly. 2 – Coding Assistance: CPT and ICD-10 Coding: Look for software that provides comprehensive support for Current Procedural Terminology (CPT) and International Classification of Diseases, 10th Edition (ICD-10) coding standards. Code Validation: The software should have built-in validation checks to ensure accurate and compliant coding practices. 3 – Revenue Cycle Management: Patient Billing: Seamless patient billing features, including invoicing, statements, and payment processing, streamline revenue collection. Denial Management: Robust denial management tools help identify and address claim denials promptly, reducing revenue loss. 4 – Reporting and Analytics: Customizable Reports: The ability to generate customizable reports based on key performance indicators (KPIs) and financial metrics is essential for monitoring practice performance. Real-Time Analytics: Real-time analytics dashboards provide actionable insights into revenue trends, claim status, and billing efficiency. 5 – Compliance and Security: HIPAA Compliance: Ensure the software is compliant with the Health Insurance Portability and Accountability Act (HIPAA) regulations to safeguard patient data. Data Encryption: Strong data encryption protocols protect sensitive patient information from unauthorized access. 6 – Integration Capabilities: EHR Integration: Seamless integration with Electronic Health Records (EHR) systems improves data accuracy and reduces duplicate entry. Practice Management Integration: Integration with practice management software ensures smooth workflows across billing, scheduling, and patient management. 7 – Automation and Workflow Optimization: Automated Reminders: Automated appointment reminders and billing notifications enhance communication with patients and improve collection rates. Workflow Automation: Automation of repetitive tasks such as claim submission, payment posting, and eligibility verification saves time and reduces errors. 8 – Scalability and Flexibility: Scalability: The software should be scalable to accommodate the growth of your practice and handle increased patient volume. Customization: Flexible customization options allow you to tailor the software to meet your practice’s unique needs and workflows. 9 – Training and Support: Training Resources: Access to comprehensive training resources, including tutorials, user guides, and webinars, ensures smooth adoption and proficiency. Customer Support: Responsive customer support services, including phone, email, and live chat support, are crucial for addressing technical issues and questions. By prioritizing these key features in your search for medical billing software, you can select a solution that optimizes revenue cycle management, enhances operational efficiency, and supports the long-term success of your healthcare practice. Benefits of Using Medical Billing Software Implementing a reliable medical billing
Common Medical Billing Errors

Common Medical Billing Errors Introduction: Efficient and accurate medical billing is essential for healthcare providers to receive timely payments and maintain financial stability. However, the complexity of medical billing processes often leads to various errors that can have significant repercussions. In this blog, we delve into ten common medical billing errors that healthcare facilities and billing professionals encounter regularly. From duplicate billing and coding errors to challenges with insurance verification and late claim submissions, each aspect plays a crucial role in the financial health of medical practices. By identifying these common pitfalls and understanding how to mitigate them, healthcare organizations can streamline their billing processes, reduce revenue losses, and enhance overall operational efficiency. Join us as we explore these ten key areas of medical billing errors and gain insights into best practices for error prevention and resolution. Let’s navigate the intricate landscape of medical billing together to ensure accurate billing, efficient reimbursement, and improved patient care outcomes. 1 – Duplicate Billing In the realm of medical billing, a formidable foe lurks: Duplicate Billing. This stealthy adversary has the potential to wreak havoc on revenue streams and reimbursements if left unchecked. In this article, we delve into the intricacies of duplicate billing, exploring how it can occur, its profound impact on financial health, and crucial strategies to fortify against its pernicious effects. Understanding Duplicate Billing Duplicate billing, at its core, involves charging a patient or insurer multiple times for the same medical service or procedure. While this may seem inadvertent, it can stem from various sources, including human error, faulty billing systems, and miscommunication between healthcare providers and billing departments. The Impact on Revenue and Reimbursements The repercussions of duplicate billing are not to be underestimated. They extend far beyond mere financial losses, striking at the heart of operational efficiency and credibility. Here are some key impacts: Financial Drain: Duplicate billing drains resources, leading to decreased revenue and increased administrative costs. Compliance Concerns: It raises compliance red flags, inviting audits and penalties that can tarnish the reputation of healthcare providers. Patient Dissatisfaction: Patients may feel aggrieved and lose trust in the healthcare system, impacting patient retention and referrals. Reimbursement Delays: Duplicate billing can cause delays in reimbursements, disrupting cash flow and hindering growth opportunities. Strategies to Prevent Duplicate Billing To combat this menace, proactive measures and robust protocols are indispensable. Here are effective strategies to prevent duplicate billing: Comprehensive Training: Provide thorough training to billing staff on coding accuracy and the importance of meticulous documentation. Utilize Technology: Leverage advanced billing software with built-in checks for duplicate claims to flag and rectify errors promptly. Regular Audits: Conduct regular audits of billing records to identify and rectify duplicate billing instances before they escalate. Enhanced Communication: Foster clear communication channels between healthcare providers, billing departments, and insurers to minimize misunderstandings. Educate Patients: Educate patients about billing processes and encourage them to review statements for accuracy, reporting any discrepancies promptly. Conclusion: Duplicate billing is a formidable challenge in the medical billing landscape, but with vigilance, education, and technological advancements, it can be mitigated effectively. By implementing robust strategies and fostering a culture of compliance and transparency, healthcare providers can safeguard their revenue, enhance patient satisfaction, and fortify their standing in the healthcare ecosystem. Remember, prevention is always better than cure, especially when it comes to safeguarding financial well-being in the complex realm of medical billing. 2 – Coding Errors In the intricate world of medical billing, accuracy is paramount. As a provider of medical billing solutions, HS Med Solution understands the challenges that healthcare professionals face when it comes to coding errors. In this blog post, we delve into common coding errors such as incorrect modifiers, unbundling, and upcoding, and provide valuable tips on how to ensure accurate coding practices. Understanding Common Coding Errors Incorrect Modifiers: One of the frequent coding errors involves the misuse or omission of modifiers. Modifiers are essential in clarifying specific details about a procedure or service provided. However, using the wrong modifier or forgetting to include one can lead to claim denials or improper reimbursement. Unbundling: Unbundling occurs when separate procedures or services are billed individually instead of bundling them together as a single code. This practice can result in overbilling and potential compliance issues. Upcoding: Upcoding involves assigning a higher-level code than what is supported by the documentation or medical necessity. This can lead to inflated reimbursements and is considered fraudulent. Tips for Ensuring Accurate Coding Comprehensive Training: Provide ongoing training and education to coding staff to ensure they stay updated with coding guidelines and regulations. Documentation Review: Emphasize the importance of thorough documentation that supports the services billed. Encourage providers to document all procedures accurately and completely. Regular Audits: Conduct regular internal audits to identify coding errors and areas for improvement. Address any issues promptly to prevent recurring errors. Utilize Technology: Leverage technology solutions such as coding software and electronic health records (EHRs) to streamline coding processes and reduce errors. Stay Compliant: Keep abreast of changes in coding regulations and compliance requirements to avoid penalties and audits. The HS Med Solution Advantage At HS Med Solution, we prioritize accuracy and compliance in medical billing. Our team of experienced professionals is dedicated to helping healthcare providers navigate the complexities of coding and billing, ensuring optimal reimbursement and regulatory adherence. In conclusion, understanding and addressing common coding errors is essential for healthcare organizations to maintain financial health and compliance. By implementing the tips outlined in this post and partnering with a reliable medical billing solution provider like HS Med Solution, providers can achieve accurate and efficient coding practices. For more information about our medical billing solutions and how we can support your practice, feel free to contact us. Stay tuned for more insightful updates on healthcare industry trends and best practices! 3 – Incomplete Documentation In the intricate realm of medical billing, the journey from patient care to reimbursement hinges on a crucial factor: documentation. Comprehensive and accurate documentation not only ensures proper patient care but also serves as
